Every patient is unique, but most clinical studies use one of the following treatment schedules:
Accepted Insurance Plans
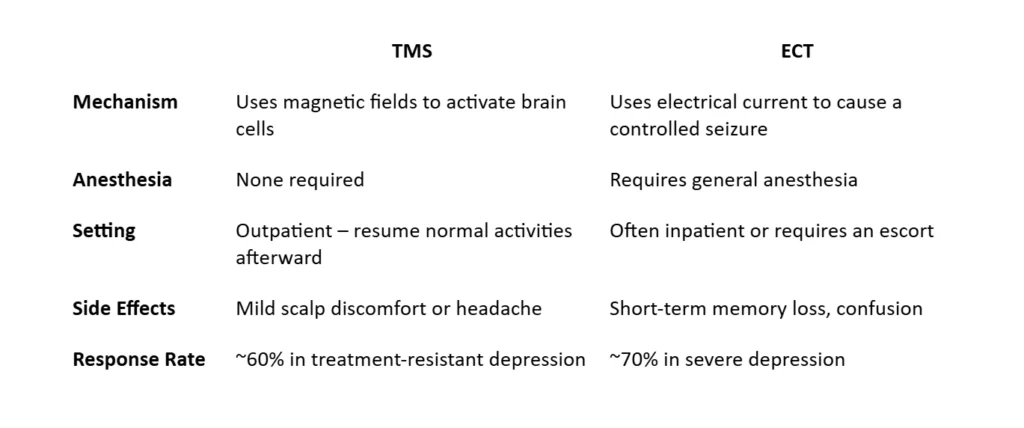
Key differences:
While response time varies, most patients begin noticing improvement after 2–3 weeks of consistent sessions (5 days per week).
Some notice changes sooner, while others respond closer to week 4–5. Early signs include better sleep, energy, and focus — followed by improved mood.
At Sleep, TMS & Wellness Psychiatry, patients receive ongoing coaching on essential wellness factors throughout their TMS treatment. This guidance focuses on improving sleep–wake cycles, establishing daily exercise routines, supporting healthy nutrition and hydration, reducing stress through a positive mindset, and strengthening social connectedness.
As part of your comprehensive psychiatric evaluation, Dr. Gupta may recommend specific medical tests to better understand the biological factors contributing to your symptoms. These assessments help guide personalized treatment decisions and ensure the safest, most effective care plan. Depending on your needs, the workup may include: